When Women Say "I'm Fine" ...... But Don't Mean It
When Women Say “I’m Fine” (And Don’t Mean It)
Because sometimes saying “I’m fine” feels safer than saying “I’m struggling.”
When I was in labor with my son, I knew something wasn’t right.
The contractions were intense and close together, but when I got to the hospital, I was told to go home — that it wasn’t time yet.
Before I even made it back home, we had to turn around and rush back to the hospital. I had my son shortly after.
That moment stuck with me — not because of the chaos of labor, but because I had known something was wrong, and still, no one listened.
The worst part? Every professional I encountered that day was a woman.
It wasn’t cruelty; it was conditioning.
These were women trained in a system that has, for decades, taught all of us to doubt women’s pain — to downplay, rationalize, and second-guess symptoms instead of trusting them.
The First Time I Tried to Tell the Truth
After my son was born, I was handed a postpartum depression screening checklist — a quick paper survey with boxes to check.
I remember hovering over my answers, scoring high, and thinking, Maybe I should actually tell the truth this time.
But as I went to leave, someone yelled my name across the waiting room, waving the paper in the air and saying, “I think we should talk.”
Everyone turned. I froze.
I felt exposed, ashamed, and suddenly desperate to backpedal. I mumbled that I’d checked the wrong boxes by accident.
That was the moment I learned that even honesty could be humiliating.
Years Later, It Happened Again
When I started college — back when I thought I wanted to be a nurse (I would’ve been a terrible nurse) — I had three kids at home and was working full-time.
I finally made a doctor’s appointment because I knew something wasn’t right.
When the medical assistant asked if I’d had suicidal thoughts, I almost said yes. But right before that, she had made small talk about the weather. I froze again. I said no.
When the doctor came in, I nervously described what I now recognize were clear symptoms of depression. She told me I was “just stressed.”
That was the last time I sought help for years.
When Women’s Health Isn’t Studied, Everyone Suffers
For years, women were systematically excluded from medical research. Hormones were considered “too complicated,” so men’s bodies became the medical default.
Even today, studies show that women make up only about 41% of clinical-trial participants despite representing more than half of the population. In early-phase drug trials, that number drops to around 30%.
And the ripple effects are huge:
- 29% of women say a healthcare provider has dismissed their concerns (compared with 21% of men).
- 93% of women aged 25–34 report feeling dismissed or not taken seriously at least once when seeking medical help.
- Heart disease — the leading killer of women — is often misdiagnosed because women’s symptoms look different from men’s, and the data used to define “classic” symptoms came mostly from male participants.
When the research doesn’t include us, the care we receive doesn’t fit us.
The Emotional Toll of Not Being Believed
I see it every week in my therapy office: women who come in feeling “crazy,” “dramatic,” or “broken” because their pain, fatigue, panic, or intrusive thoughts were minimized by a professional.
They describe sitting on exam tables rehearsing their words, afraid of being labeled “pill-seeking” for simply asking for relief.
They minimize their pain so they don’t seem “difficult” or “attention-seeking.” They apologize for advocating for themselves.
They leave appointments in tears — not just because they didn’t get answers, but because they left feeling invisible.
This is not a lack of resilience. It’s a trauma response — the nervous system’s way of saying, You’re on your own again.
Our Bodies Aren’t the Problem — The Stigma Is
The irony is that much of what women experience as “moodiness,” “fatigue,” or “irrationality” is actually biology doing its job.
Our bodies are most regulated in the week after menstruation, when estrogen rises and supports mood, focus, and energy.
The week before our period, estrogen drops and progesterone increases — heightening emotional sensitivity, anxiety, and physical discomfort.
That’s not weakness. That’s physiology.
But instead of being understood as natural hormonal rhythms, these changes are often stigmatized — turned into punchlines (“must be that time of the month”) or dismissed altogether (“you’re overreacting”).
When your body fluctuates every month but the world expects you to stay the same, it’s easy to feel broken.
You’re not. You’re cyclical in a culture that only values consistency.
Anxiety Isn’t the Problem — It’s the Messenger
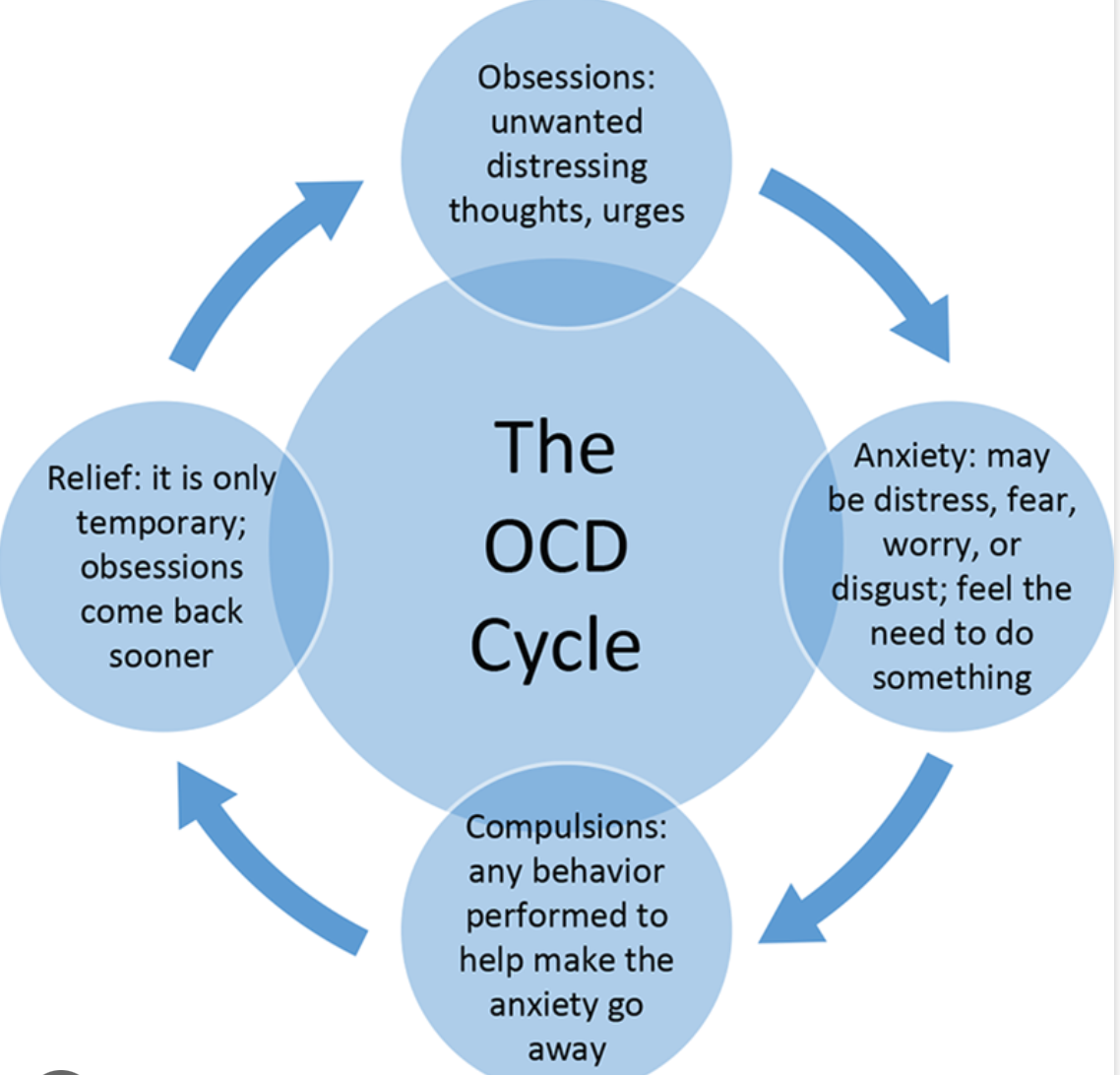
When your body keeps sending signals that something’s wrong and those signals are ignored, anxiety becomes the only language left.
Anxiety says: Pay attention.
The system says: Calm down.
And you end up stuck between the two, feeling both unheard and unsafe.
Anxiety isn’t your enemy — it’s the body’s alarm system trying to get through a world that keeps muting it.
When women’s symptoms are minimized, our anxiety often grows louder — not because we’re fragile, but because our bodies are begging to be believed.
What Needs to Change
- More inclusive research. Clinical trials, diagnostic tools, and medication studies must represent women’s physiology — including hormonal shifts, postpartum changes, and autoimmune responses.
- Bias training in medical education. Dismissal isn’t just about compassion; it’s about conditioning. Professionals need to unlearn the reflex to minimize women’s pain.
- Validation as intervention. When a woman says, “Something’s wrong,” the most powerful response is, “Tell me more.”
For the Women Reading This
If you’ve ever left an appointment feeling small, dismissed, or crazy — you weren’t. You were trying to be heard in a system that wasn’t built to listen to you.
You don’t have to prove your pain to deserve care. You don’t have to stay quiet to be believed.
Your anxiety isn’t broken. It’s begging to be believed.